Your COVID-19 Testing FAQs Answered
If you have more questions than answers about COVID-19 testing, you’re not alone. Employers want to know if employees can be tested before returning to work. Employees who fear they have been exposed or may be getting sick want to know if, when and where they can get tested.
Like so much else these days, testing availability and protocols are in flux. To help employers understand the current status in the US, we’ve gathered and summarized information available from the CDC and other public resources. We’ll provide an overview of current testing availability and protocols, and offer some answers to questions we’ve been hearing from employers. We’ve also created a flowchart that you can share with employees that should answer many of their questions about if, when and how to seek testing. Remember, the situation is changing weekly, if not daily. This information is valid as of March 25th. Check the CDC and state health departments for the latest information.
TESTING AVAILABILITY
The U.S. is still far behind countries with the most aggressive testing programs, like China and South Korea. Although we are seeing significant progress in expanding availability, testing in most communities is still limited and prioritized.
State and local public health laboratories in all 50 states have verified COVID-19 diagnostic tests and are offering testing. Specimens must be collected by a healthcare provider and submitted to the public health lab for processing. Many state and local public health entities across the country are opening drive-up collection sites for testing. Most are requiring a written or printed physician order to be in hand before an individual arrives at a drive-up site and collection is performed. Procedures vary, but some ask patients to fill out forms or to take an online assessment prior to arriving; some require that a clinician complete an assessment of testing necessity.
Testing in private labs is ramping up; LabCorp and Quest have announced that they expect to be conducting 140,000 - 280,000 tests per week by April 1st in locations all over the country. This addition should make testing significantly more accessible. At this time, these labs are running specimens but not collecting them. Specimens must be collected by a healthcare provider and sent to the lab for processing.
Home test kits are being marketed direct to consumers (and employers). While there is obviously huge demand, and some would say a pressing need, for at-home testing, at this time they should be discouraged. Most importantly, the test quality is unknown and it is not clear that individuals will get adequate samples, which can be technically difficult. In addition, information about results will not be part of the administrative data set since no claim will be filed. The FDA issued a strong statement last week that they have “not authorized any test that is available to purchase for testing yourself at home for COVID-19.” However, they also said that they see the value of at-home testing and are “actively working with test developers in this space.”
WHO CAN GET TESTED?
State and local guidance varies significantly and is at least somewhat dependent on existing, current resources and testing availability, prevalence of COVID-19 and rate of community spread. Some states, including WA, MN and DC, advise healthcare providers to test any patient with symptoms consistent with COVID-19 (fever, cough, shortness of breath). Other states, including CO and TX, have tougher criteria: symptoms consistent with COVID-19 plus exposure and/or risk factors including age and/or existing medical conditions.
The CDC is advising that as private lab testing becomes more widely available, clinicians should consider testing a wider group of symptomatic patients. Currently, however, mildly ill patients should be encouraged to stay home and contact their healthcare provider by phone for guidance about clinical management. Patients who have severe symptoms, such as difficulty breathing, should seek care immediately. Older patients and individuals who have underlying medical conditions or are immunocompromised should contact their physician early in the course of even mild illness.
Testing those with no symptoms (with an exposure history or simply concerned) and those with mild symptoms is typically not recommended.
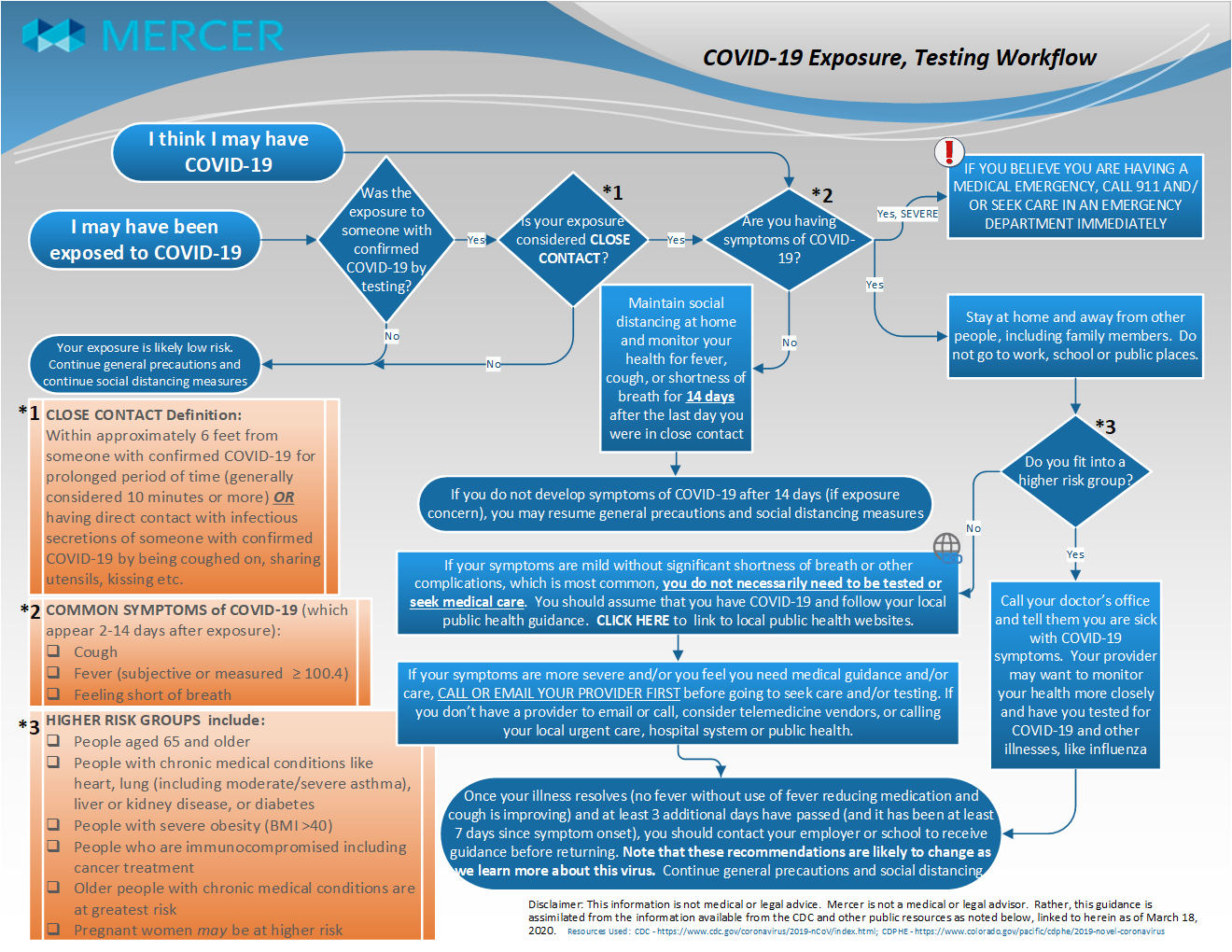
*Click to download image
EMPLOYER FAQS (These answers are based on guidance from the CDC.)
How do I know if an employee was exposed?
If an employee had close contact with someone known to have COVID-19, he/she would be considered as having been exposed. Close contact is defined as:
- Being within approximately 6 feet of a known (confirmed by testing) COVID-19 case for a prolonged period of time (which can generally be considered as 10 minutes or more), or
- Having direct contact with infectious secretions of someone with known COVID-19 (e.g., being coughed on, sharing utensils or kissing)
Living in the same household as, being an intimate partner of, or caring for a person with symptomatic laboratory-confirmed COVID-19 infection, is also considered an exposure according to the CDC. More information on exposure risk is available from theCDC.
What should I do if an employee has been exposed but is not sick?
The employee(s) should be sent home and advised to stay at home. They should monitor their health for fever, cough, or shortness of breath for 14 days after the last day they were in close contact with the sick person with COVID-19. After the 14-day period, if no symptoms develop, employee(s) who were exposed can return to work.
What should I do if an employee develops symptoms of COVID-19 such as cough and fever?
- Employee(s) who become sick with symptoms of COVID-19 should be advised to stay at home and away from other people. Sick employees should be advised not to come to work, and avoid public places until their symptoms have completely subsided and at least 10 days have passed. Keep in mind that they may still be contagious for a time even after their symptoms have subsided, so precautions should be taken accordingly.
- If employee(s) is/are at higher risk of getting very sick from COVID-19, they should be advised to contact their doctor’s office and tell them they were exposed to someone with COVID-19 and are having symptoms.
- Employees should not be asked to provide a doctor’s note before returning to work. Providers will be busy caring for sick patients. Your procedure for returning employees who were sick with COVID-19 may vary, and it is imperative to check with your local health department and/or the CDC for the latest guidance in this regard. The CDC has provided the following guidance for when employees who were sick at home (i.e. not hospitalized) with COVID-19 may discontinue home isolation:
- At least 3 days (72 hours) have passed since recovery defined as resolution of fever without the use of fever-reducing medications and improvement in respiratory symptoms (e.g., cough, shortness of breath); and,
- At least 7 days have passed since symptoms first appeared.
Note that the above recommendations are likely to change as we learn more about this novel virus.
Some final reminders
- Stay home if you’re sick. At this point in time, anyone with a fever and cough should assume their illness could be COVID-19 and take steps to protect others in the community and household from the disease.
- Call first. If employee(s) have symptoms of COVID-19 or believe they may have been exposed, advise them to call or emaila health care provider first. Employees should be advised not to go to an emergency room to get a test for COVID-19 unless they are having a medical emergency.
- Dial 9-1-1 for medical emergencies. Employees should be advised to call 911 or go to an emergency room if they are having a medical emergency. For COVID-19, that means severe respiratory symptoms such as shortness of breath or difficulty breathing.
If you have additional questions about testing or other COVID-19 topics, contact your Mercer consultant or join one of our weekly webinars.
