Thinking Big: Network Strategies to Drive Better Performance

They’re also managing their out-of-network spend. Even though federal lawmakers are focused on policies to protect consumers from surprise medical bills, jumbo employers are pushing ahead with strategies to eliminate OON coverage, except for emergencies and other network deficiencies. Seven percent have eliminated OON coverage entirely with another 25% considering this step.
With these networks strategies, jumbo employers that I’ve worked with are realizing savings of as much as 15% over a traditional PPO. To do this, they’ve been willing to put in the effort to quilt together a network and implement approaches that are different from the status quo. They understand that provider disruption is no longer the most important decision point when evaluating a network strategy. Focusing on how to better align the plan to drive better performance will result in significant and long-lasting benefits for their organization and employees.
Each year, when we review the results of our National Survey of Employer-Sponsored Health Plans, we eagerly look to see what the nation’s largest employers are doing and planning, since this group is where many of the innovators, trendsetters and early adopters are to be found. Employers were asked to indicate their most important strategies for the next five years and, not surprisingly, managing cost for specialty pharmacy and managing high-cost claims were cited as very important or important by the most jumbo employers (89% and 84%, respectively, of those with 20,000 or more employees). But I was most interested to see that for fully half of these employers, high-performance network strategies will be important over the next five years.
To me, it’s good news that employers are embracing disruption in their health plan networks. In my blog post – Three Steps to Building a Better Health Plan Network – I recommended employers start by sizing the opportunity. As we found in a follow-up survey of 227 very large employers, not only are they sizing the opportunity, they’re quilting together the best options by location to drive employees to ACOs and other high performance networks that better manage cost and achieve higher quality care.
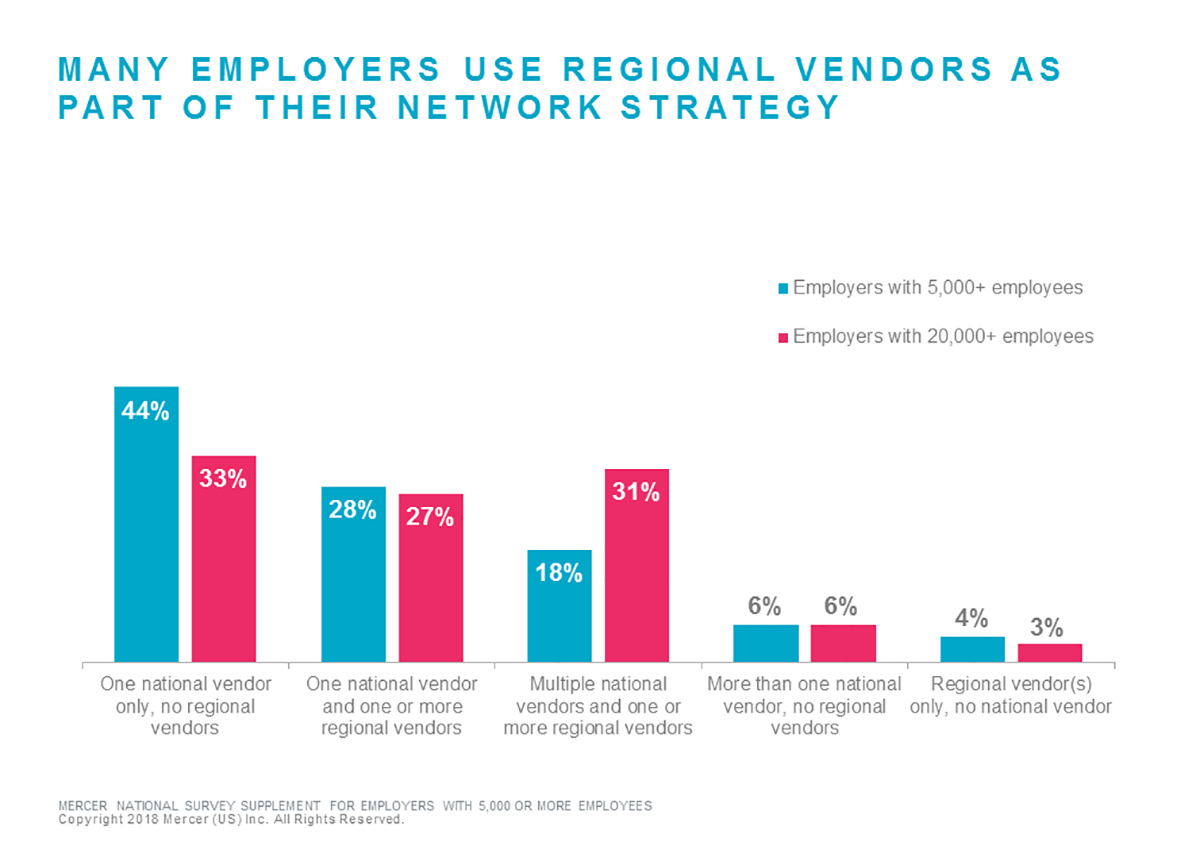
So how are they doing it? Over half of the jumbo employers surveyed (57%) use one or more regional health plan vendors in addition to a national vendor, and a handful (3%) use only regional vendors. Of the employers using one or more regional vendors in addition to (or instead of) a national vendor, the top three reasons are: deliver best cost / savings (69%); meet employee access needs (57%); and drive employees to health systems with better cost management and care quality (55%).
Related products for purchase
Related Solutions
Related Insights
-
US health newsAI-assisted research is turning up some interesting uses for mammogram imaging beyond screening for breast cancer.
-
US health news
PSYPACT gets an A (for access, among other things)
Learn how the Psychology Interjurisdictional Compact (PSYPACT®) may benefit employers as they seek to improve employee mental health. -
US health news
Treating severe mental health disorders with psychedelic substances
James deSpelder discusses the potential uses and concerns of using psychedelics to treat mental health issues.









