New Transparency Rule Requires Plan Sponsors to Disclose Costs Up Front
In the waning days of his first term, the Trump Administration delivered final regulations that will require most group health plans and insurers to disclose price and cost-sharing information. President Trump has long been a proponent of increasing competition in healthcare. In a rule finalized last year, hospitals are required to make their standard charges publicly available beginning in 2021. Despite legal challenges to enjoin the rules, it appears the rule will go into effect as written.
The Transparency in Coverage rule has a phased in implementation that would require plan sponsors and insurers for plan years beginning on or after:
- January 1, 2022 release of three separate machine-readable files that include detailed pricing information of all in-network negotiated rates, historical payments and charges from out-of-network providers, and prescription drug in-network negotiated rates and historical net prices at the pharmacy location level.
- January 1, 2023 disclosure of out-of-pocket cost information and the underlying negotiated rates through an internet-based self-service tool for 500 shoppable services as determined by the Administration.
- January 1, 2024 disclosure of price and cost-sharing information for all items and services through the self-service tool.
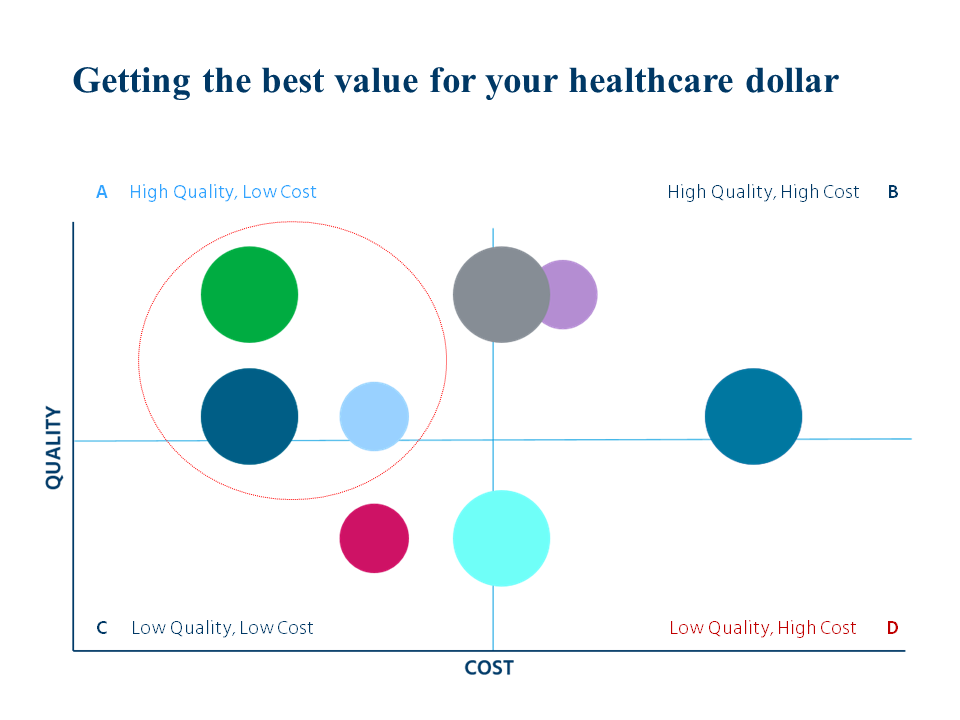
A couple of noticeable changes from the proposed rules are the separate machine-readable file for prescription drug prices and the phased effective dates. We certainly welcome the effective date relief. While not specifically requiring a quality metric, the regulators may address that in future guidance and encourage plans and issuers to further innovate around the baseline transparency standards and include quality information and other metrics that would assist in consumer decision-making. As we’ve said before quality matters, especially for more complex care – it means fewer complications, better outcomes and lower overall costs. But hey, we have to start somewhere.
Make no mistake; this is a heavy lift for employer-plan sponsors who will need to work with their health plan partners to obtain the data they need to disclose the data. In their haste to comply with the regulations employers may miss a golden opportunity. This is the time to put quality front and center.
We’ve been working hard on a tool that can help bring transparency to employer health plan strategy. QualPic is Mercer’s proprietary database tool that functions as a diagnostic in markets across the country, helping paint a picture of cost and quality for different categories of care, ranging from primary care to orthopedics and more. By looking at consistent metrics across markets, employers can start to understand the amount of variation in healthcare cost and quality from one location to the next. The practical application of this information is identifying and quantifying savings opportunities in shifting care from some providers to others.
For too long, we’ve accepted the excuse that measuring quality in healthcare is just too hard. It’s 2020, and with data science on our side, we’re ready to turn this conversation into action. Let’s get started!


