Measure Health as a Bellwether of Equity

Findings from our new study on racial workplace disparities “Stepping Up for Equity” show that many companies have yet to begin to leverage data on race and ethnicity to uncover health disparities in their populations. While many have initiatives underway to achieve equity in pay and career opportunities, when it comes to the critical issue of health and well-being there is much more that could be done.
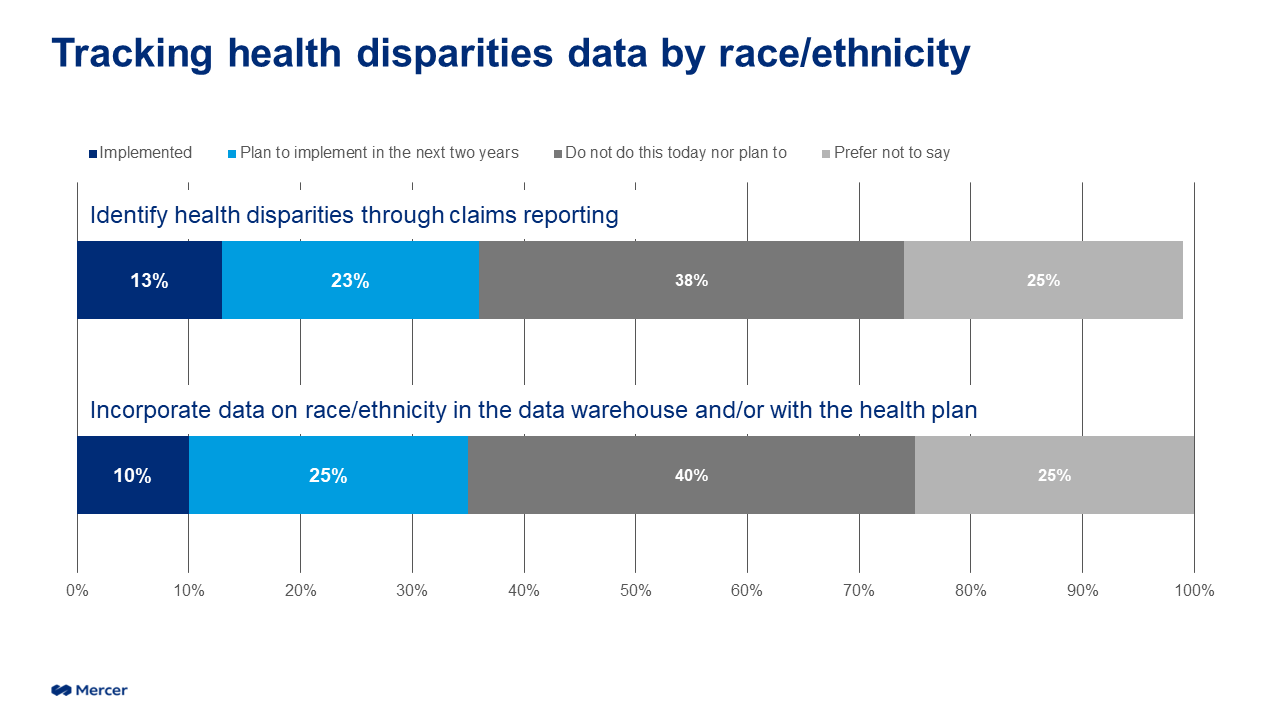
To start, employers can begin tracking aggregated and de-identified health claims and risk data through the lens of race/ethnicity. Our survey shows that only 10% of respondents currently include information on race/ethnicity in their claims data, although another 25% have plans to do so.
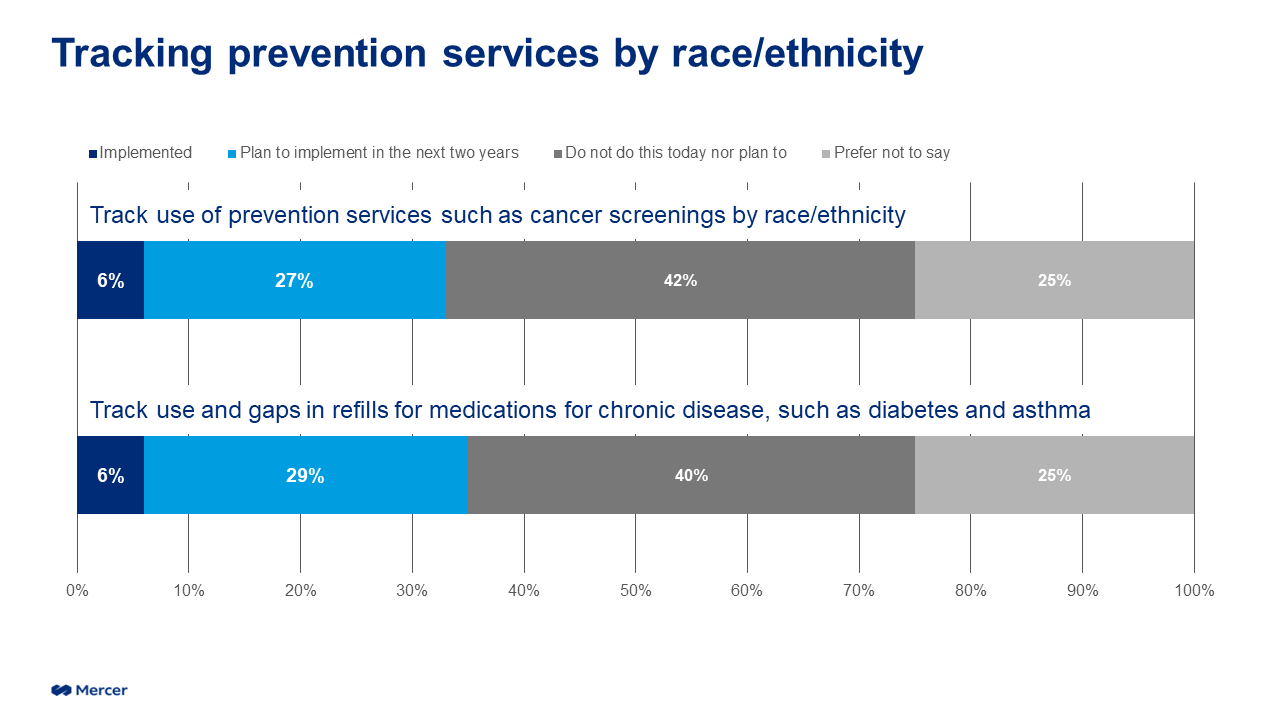
We know that preventive measures, such as screenings for cancer — as well as services for chronic conditions, such as refilling medications — are important components that support a healthy and productive workforce. While few respondents – just 6% – currently track either prevention services or prescription refills by race/ethnicity, it is encouraging to see that a substantial number plan to begin within the next two years.
The easiest way to obtain reporting by race/ethnicity is to have employees self-identify and then provide that data to the carriers via employer eligibility files. In our recent carrier request for information, 68% of respondents indicated they could provide health disparity reporting if this data is provided. And for even more robust reporting, employers should ask carriers to analyze ICD-10 Z-code data. Health providers use Z-codes to document social, environmental and economic factors that impact a patient’s health outcomes. These codes can be used to identify health disparities and track progress over time. Unfortunately, only about 2% of claims have Z-codes attached. Employers should press health plans to do more to increase their providers’ use of Z-codes.
Once organizations have the data to identify health disparities, they can implement targeted programs — in conjunction with their benefit vendor partners — focused on improving healthcare experiences and outcomes for Black employees and other underserved populations. This includes health equity initiatives and targeted wellness programs based on race/ethnicity. Employers are in a unique position to partner with health plan administrators and even healthcare systems to improve health equity. This could take several forms:
Provider diversity: Make available information about the race, ethnicity, etc., of healthcare providers, collected on a voluntary and self-identified basis, to allow members to find providers who look like them and share their lived experience.
Cultural competency and cultural humility training for healthcare providers and teams: More health plans offering training on cultural competency and cultural humility for providers and healthcare teams may help improve the member experience and potentially health outcomes.
Verticalized navigators/digital health solutions: These are emerging solutions designed to address specific needs of the Black and other under-served population that may not otherwise be covered adequately by the employer’s primary health plan.
Value-based care: Some published studies show that value-based care arrangements, such as centers of excellence, have demonstrated improved health outcomes and member experience.
Social determinants of health (SODH): Some employer-sponsored plans are beginning to identify social risks, assess for social needs and offer coordination to community-based organizations (CBOs) to meet those needs. Black employees, as well as other under-served populations, are disproportionately impacted by SDOH and have a greater need for services from CBOs.
Employers have a tremendous opportunity to move the needle on DEI. Supporting employee well-being is top of mind for most employers as we emerge from the pandemic, and it makes sense to focus efforts on Black employees and other underserved populations that have long experienced health disparities. The first step is simple: Get the data you need to take action.
